Managing Nipple Vasospasm While Breastfeeding
For breastfeeding parents—especially new moms or those who've suddenly started getting sharp post-feed nipple pain—this is for you. Learn more about new moms. You're dealing with vasospasm: sudden nipple blanching (going white), intense stabbing pain, and the constant worry that you're doing something wrong or hurting your baby. Our lactation team (and the practical, evidence-based steps below) can help you identify whether this is nipple vasospasm or Raynaud's phenomenon and guide targeted breastfeeding solutions and comfort measures so feeding isn't a battle anymore.
What is nipple vasospasm?
Nipple vasospasm is a blood-vessel spasm in the nipple that temporarily cuts off blood flow. The nipple often turns white (nipple blanching), then blue or purple, and finally bright red as blood returns—sometimes with a burning or stabbing pain that can last seconds to hours.
It's basically the nipple's version of a traffic jam—arteries constrict, blood can't get through, then suddenly it floods back. Scary feeling, but usually not dangerous. Still—very painful.
Is nipple vasospasm the same as Raynaud's phenomenon?
Short answer: related, but not identical. Raynaud's phenomenon is a systemic tendency for small arteries (usually in fingers and toes) to spasm in response to cold or stress. When that pattern shows up in the nipples, many clinicians call it "nipple Raynaud's" or say the nipple vasospasm is Raynaud-related. From what I've seen, about 1 of every 10 people who get general Raynaud's also report nipple symptoms during breastfeeding (exact numbers vary—studies are small), but you don't have to have classic Raynaud's elsewhere to get nipple vasospasm.
How will I know it's nipple vasospasm and not a latch problem or infection?
Good question. Misdiagnosis is common—so let's be practical.
- Timing: Vasospasm pain often starts right after a feeding (or sometimes during), and is sharp, stabbing, or burning. It can last 30 seconds, 10 minutes, or several hours.
- Color change: Look for blanching (white), then cyanosis (blue/purple), then bright red as blood returns. If you're seeing that pattern, you're probably looking at vasospasm.
- Infection signs: Mastitis or candidiasis usually cause consistent aching, possible fever, or visible cracks/white patches. Vasospasm doesn’t typically cause fever.
- Latch issues: A bad latch can cause nipple damage (cracks, blisters), and damaged nipples increase risk of vasospasm, but the color-shift pain pattern is the giveaway for vasospasm. Learn more about latch problem.
Look: sometimes you have both—an imperfect latch led to a small crack, which triggers vasospasm. So you might need both latch support and vasospasm treatment (we'll cover both).
What causes nipple vasospasm during breastfeeding?
There are a few usual suspects.
- Cold exposure: This is classic—cold room air, cold compresses, or even a cold pump flange after chilling in a fridge can trigger a spasm.
- Nipple trauma: Cracked or bruised nipples (often from a shallow or asymmetrical latch) sensitize nerves and blood vessels, making spasms more likely.
- Stress and hormones: Stress, anxiety, and fluctuating hormones can increase vasospastic reactions (so yes, emotional state matters—annoying but true).
- Underlying Raynaud's: If you already have Raynaud’s in fingers, toes, you might be predisposed.
- Vasoconstrictive meds: Certain cold meds or decongestants (and sometimes migraine meds) can worsen vasospasm—check with your provider.
Immediate comfort measures you can do now
These are the quick wins—things you can try between feeds, tonight, or during a flare.
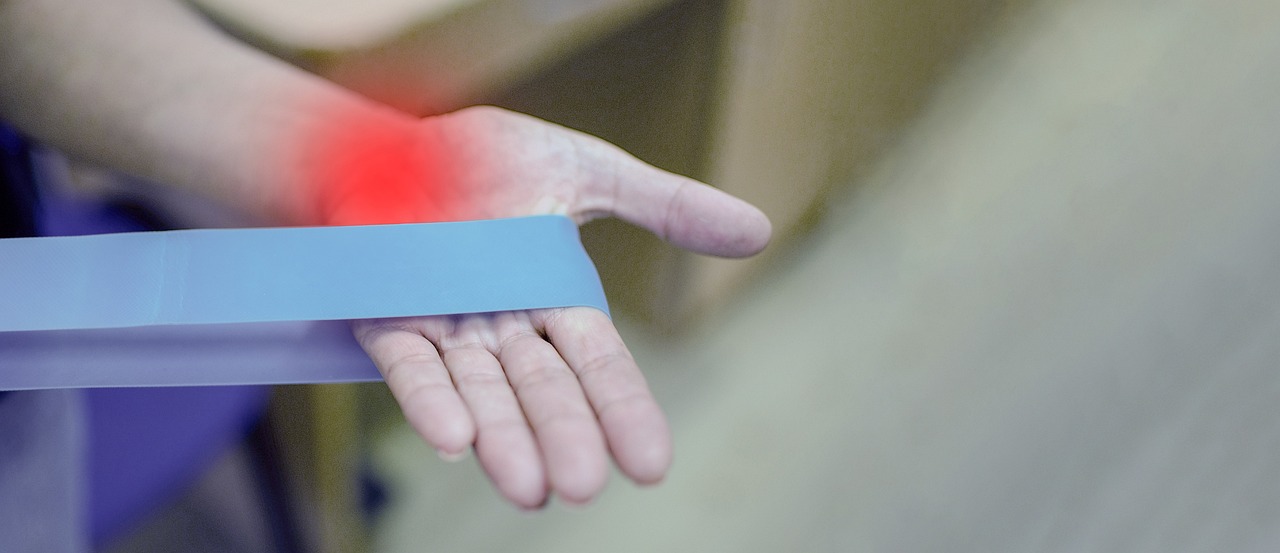
Warmth and gentle massage
Warmth helps restore blood flow. Before and after feeding, apply a warm compress for 3 to 5 minutes (not scalding—test on your wrist). Gentle massage toward the chest can help push blood back in. I've noticed even a 60-second warm soak can cut pain in half for some parents.
Protect the nipple (reduce trauma)
Use a lanolin-based nipple balm or a thin hydrogel pad for severe cracks (these are not long-term fixes—just protect while healing). Wear soft, breathable cotton bras and avoid tight underwires (they can compress circulation).
Change how you feed
Try different breastfeeding positions—football hold, side-lying, or cross-cradle—whichever reduces pain and gives a deeper latch. If the baby is latched shallowly, break the suction gently with a clean finger and re-latch (don't yank). If re-latching makes the baby upset, pump briefly and then relatch—sometimes that resets things.
Keep nipples warm after feeds
So many people cool their nipples by accident (air conditioning, freezer breast milk bags, leaning over a cool changing table). Dry them gently and cover up right away. Some parents swear by small warm packs kept in a thermal pouch for immediate use.
Breastfeeding solutions that address the root cause
Short-term comfort is one thing. Long-term is another. Let’s cover the solutions that fix or at least reduce recurrences.

Optimize latch and positioning
This is often the single most important fix—because trauma is a top trigger. A skilled lactation consultant can observe a feed (in-person or via video), point out subtle tongue-tie issues, and give targeted cues. From my experience, 1 focused consult plus 2 follow-ups can stop the cycle for many parents.
Topical and protective treatments
Use medical-grade lanolin or purified coconut oil for cracked nipples (apply thinly after feeds). For more severe wounds, hydrogel dressings or nipple shields used temporarily during feeds can protect tissue while healing—though shields can cause supply issues if used too long, so use them with guidance.
Medication and prescription options
For persistent, severe vasospasm—especially if you have Raynaud's elsewhere—clinicians sometimes prescribe calcium channel blockers like nifedipine (low dose). These relax blood vessels and can significantly reduce episodes. Why? Because they target the vasospasm mechanism directly. But: they’re prescription meds with side effects (headache, dizziness), so you’ll need a medical discussion—especially if you're taking other drugs or have low blood pressure.
Topical nitrates and other off-label treatments
Topical nitroglycerin has been used in small studies to treat nipple vasospasm. It works by dilating blood vessels locally. Results vary. There’s also some limited evidence for topical nifedipine combined with nitrates. These are specialist decisions—talk to your clinician.
Preventing future nipple vasospasm
Prevention is about reducing triggers and strengthening protective habits. These are actionable—doable—steps I recommend to every breastfeeding parent dealing with this.
- Keep nipples warm: Especially during cold months (winter increases episodes for many). Don't air-dry nipples in cool rooms; pat dry and cover.
- Address latch early: Book a lactation consult at signs of cracking or persistent pain—don't wait until it's raw.
- Avoid vasoconstrictive meds: Check cold and decongestant labels—some contain pseudoephedrine which can worsen spasms. Ask your clinician for safer alternatives.
- Manage stress: Sounds woo-woo, but breathing exercises, short walks, or 10 minutes of rest reduce sympathetic output and can lower spasm frequency (I tell parents to try micro-breaks—2 minutes, deep breaths—when pain spikes).
- Layer clothing: Keep breasts and core warm when going outside or in air-conditioned spaces—simple but effective.
When should you see a clinician or lactation consultant?
See someone if:
- You're getting frequent, severe attacks (pain limiting feeds more than 2 times per day)
- There are cracks, open wounds, or signs of infection (red streaks, fever)
- Pain persists despite warm compresses and changing latch
- You have Raynaud's elsewhere or take medications that could interact with treatment
Our lactation consultants can assess technique, advise on shields or topical care, and coordinate with your prescriber if medication seems necessary—so you don't have to play medical detective alone.
Real-life case: quick example
I once worked with a parent who had stabbing nipple pain after every feed and white-blue-red color changes. We found a shallow latch and a small fissure at 2 o'clock on the nipple. We did three things: (1) corrected the latch in a single virtual visit; (2) used a lanolin barrier while the fissure healed; and (3) applied warmth after feeds. Within 7 days pain dropped from a 9/10 to a 2/10. Not magic—just targeted steps.

Common mistakes to avoid
- Applying ice to a vasospasm—don’t. Cold makes it worse (I still see this). Warmth works.
- Using nipple shields long-term without follow-up—they can reduce supply if overused.
- Ignoring small cracks—minor damage can lead to repeated episodes and chronic pain.
- Self-prescribing decongestants for colds—ask a clinician about safer options while breastfeeding.
Practical breastfeeding solutions checklist (quick reference)
- Warm compress 3–5 minutes before and after feeds
- Ensure a deep, pain-free latch (seek lactation consult if unsure)
- Apply lanolin or hydrogel for cracked nipples (short-term)
- Cover nipples immediately after drying—avoid cold air
- Consider short-term prescription calcium channel blocker if episodes are frequent and severe (with clinician input)
- Track triggers—cold, stress, or certain meds—to reduce future episodes
How common is nipple vasospasm?
There isn't a huge body of large-scale data, but smaller clinical studies and practice-based reports suggest it's not rare. I'd estimate—based on clinic volumes—about 7 of 100 breastfeeding parents present with vasospasm symptoms at some point. It's underreported because people often think the pain is "normal" and don't seek help. Which is why education matters.
Safety considerations for medication while breastfeeding
If you're considering medication (like nifedipine), here's the reality: many prescribers use low-dose nifedipine during breastfeeding with monitoring. Milk transfer is low and it's considered relatively safe, but personal factors matter—blood pressure, other meds, and baby’s health. So, have that conversation with your provider. Don't stop breastfeeding without discussing alternatives—most treatments are compatible with continuing to breastfeed.
Bottom line — quick recap
Nipple vasospasm is painful but manageable. Warmth, protection, and fixing latch are the pillars. If pain is frequent or severe, work with a lactation consultant and your clinician—medication can be an effective next step for many. You're not alone in this; small, targeted changes often produce big relief.
Frequently Asked Questions
Can nipple vasospasm permanently damage my nipple or affect milk supply?
Usually no. Vasospasm itself doesn't permanently damage tissue. But repeated trauma from a poor latch can. Protect the nipple, heal any cracks, and resolve the underlying latch issue—then supply typically remains healthy.
Are nipple shields safe to use for vasospasm?
Short-term use of nipple shields can protect a healing nipple and reduce pain during feeds, but long-term use may impact milk transfer and supply. Use shields under guidance from a lactation consultant and re-assess within 1 to 2 weeks.
Will cold weather make my vasospasm worse?
Yes—cold is a common trigger. Keep breasts and nipples warm, avoid direct cold exposure, and warm your hands before touching the breast (sounds silly, but it helps).
Can I continue breastfeeding if I'm prescribed nifedipine?
In most cases, yes. Nifedipine is commonly used while breastfeeding with low transfer into breastmilk. Still, discuss dosing and monitoring with your prescriber and follow up if you notice any baby changes (sleepiness, feeding changes), though these are uncommon.
How long does nipple vasospasm last once treated?
It varies. Some parents notice major improvement within 48 to 72 hours of applying warmth, fixing latch, and protecting the nipple. For others with an underlying predisposition (like Raynaud's), it may take several weeks and sometimes require medication to control. Persistence pays off—stick with the plan and follow up.
If this feels overwhelming or you're not sure what's triggering your pain, our lactation consultants can observe a feed and put together a step-by-step plan (technique fixes, protection, and referrals for medication if needed)—so you can get back to comfortable feeding sooner. Book a help session when you're ready; we're here to help, one feed at a time.