Diastasis Recti and Breastfeeding: What You Need to Know for Postpartum Recovery
For new parents (especially breastfeeding moms) who notice a soft midline or gap in their belly after delivery: you're probably worried about whether diastasis recti will affect nursing, how to fix abdominal separation, and when it's safe to rebuild core strength without making things worse. You're not alone — many people feel overwhelmed, confused by mixed advice, and nervous about exercising while breastfeeding. Our postpartum specialists (pelvic floor physical therapists and lactation-aware trainers) can guide you step-by-step — from safe breastfeeding positions to targeted rehab — so you recover function, reduce pain, and feel like yourself again. Learn more about postpartum recovery.
What is diastasis recti and why does it matter for breastfeeding?
Diastasis recti is a separation of the two halves of the rectus abdominis (the "six-pack" muscle) caused by stretching of the linea alba, the connective tissue between them. It's common after pregnancy because the belly stretches to accommodate a growing baby. Not cosmetic only — it affects posture, pelvic stability, and core strength, which all matter when you're carrying and nursing an infant.
Now, does diastasis recti stop you from breastfeeding? Short answer: no. But it can make breastfeeding more uncomfortable (back pain, poor positioning), and it can slow your overall postpartum recovery if you ignore core rehab.
Can diastasis recti affect my breastfeeding posture or comfort?
Yes. Here's how.
- Poor core support can cause you to slump (rounded shoulders), which makes nursing positions uncomfortable and may increase nipple trauma because baby struggles to latch well. Learn more about struggles to latch well.
- Weakness in the front core often coexists with pelvic floor dysfunction — that can change how you hold baby and the amount of time you can comfortably nurse.
- Some moms compensate by gripping their baby with one arm and twisting their torso, which leads to neck and shoulder pain (ugh).
How do I check for abdominal separation at home?
Quick self-check (do this when you're lying flat, knees bent):
- Place one hand behind your head and the other on your belly above the belly button.
- Lift your head just like doing a small crunch and feel along the midline for a gap.
- Measure gap width by counting finger-widths — 2 or more finger-widths often indicates diastasis recti (but clinical assessment is best).
I've noticed many people mistake general flabbiness for separation. So, if you find a gap, get a professional check (pelvic PT or OB/GYN) — they can measure depth and tissue quality, which matters for treatment.
When can I start healing my core while breastfeeding?
Short answer: As soon as you feel ready. There's no one-size-fits-all timeline.
Right after birth you should avoid intense abdominal strain (no heavy lifting, no crunches). But gentle activation — like diaphragmatic breathing and pelvic floor engagement — can begin within days. Why? Because early neuromuscular re-education helps retrain your system and prevents compensations.
Safe early moves (you can do while nursing)
- Diaphragmatic breathing: inhale to expand ribs, exhale and gently draw the lower belly in (10 breaths, multiple times/day).
- Pelvic floor squeezes: 5 seconds on, 5 seconds off, 10 reps — do them between feeds.
- Transverse abdominis activation: think "zipping up" from pubic bone to belly button (gentle, not a full crunch).
Which exercises should I avoid with diastasis recti while breastfeeding?
Don't do forceful abdominal moves that spike intra-abdominal pressure — no crunches, sit-ups, heavy deadlifts, or double-leg lowers early on (and honestly, not until a pro clears you). Movements that cause a visible bulging or coning at the midline are red flags.
What exercises help rebuild core strength safely?
Focus on quality, not quantity. Here are practical progressions I've used with clients:
- Phase 1 (gentle): diaphragmatic breathing + pelvic floor + TA activation while lying and seated.
- Phase 2 (integrative): heel slides, modified bridges, bird-dogs with core bracing (6–12 weeks, depending on healing).
- Phase 3 (functional): loaded carries, squats with proper bracing, progressive plank variations — only after a PT clears you and you can hold a neutral midline under load.
Remember: do fewer reps with better control. I'd rather see someone do 5 perfect reps than 50 sloppy ones.
How does breastfeeding itself influence recovery?
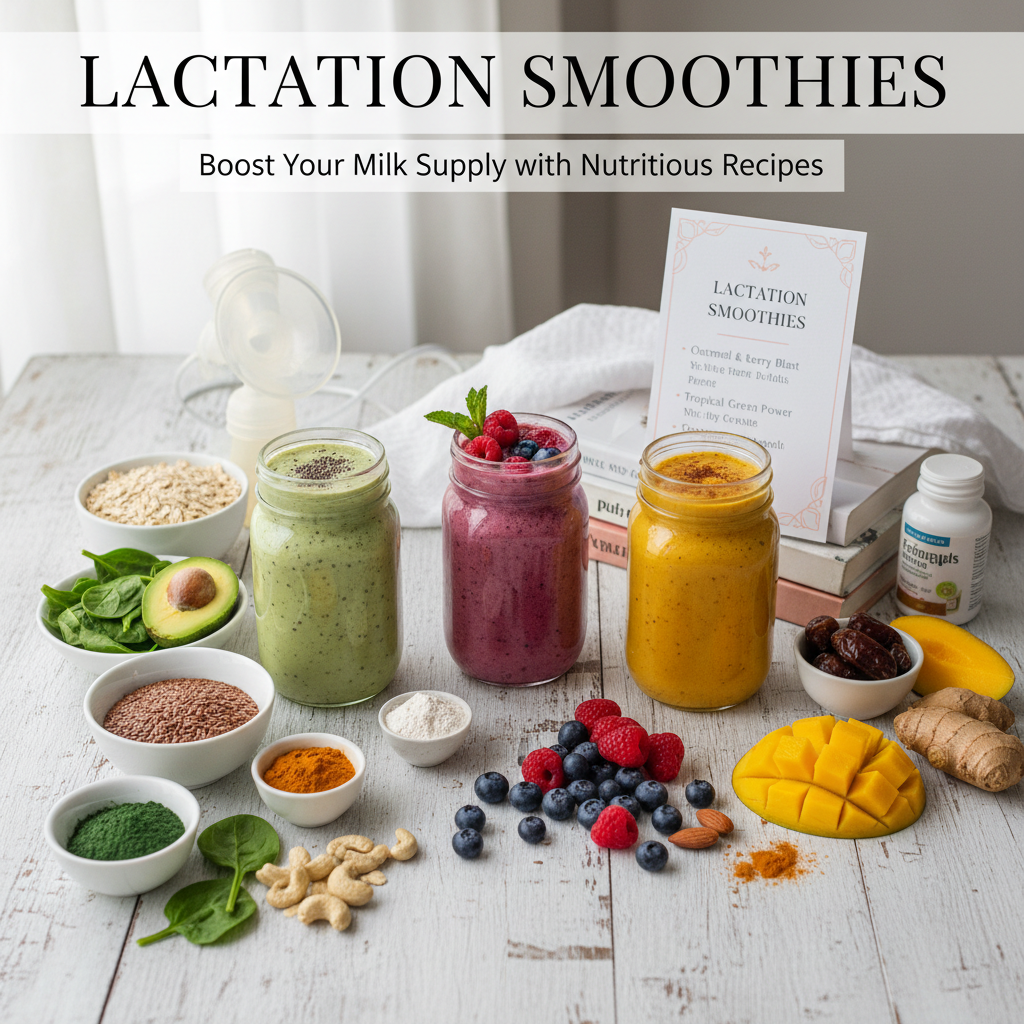
Breastfeeding releases oxytocin and prolactin — hormones that help bonding (and uterine contraction). But there's also sleep disruption, high demands on posture, and occasional nutrient depletion. So, your healing can be slowed by fatigue and poor nutrition.
Eat protein-rich meals, hydrate, and sneak in short rest breaks (even 10 minutes helps). If you're low on iron or vitamin D, get labs checked — I've seen 1 in 6 clients with deficiencies that slowed energy and recovery.
Practical breastfeeding tips if you have diastasis recti
- Use pillows to support baby so you're not leaning forward — a proper neutral spine reduces strain.
- Try side-lying or laid-back positions (biological nurturing) — they often reduce core engagement and are easier on the midline.
- Wear a supportive nursing bra and consider a postpartum belly support for short periods (not all day) — it can help during feeding marathons.
- Rotate positions so one side doesn't overwork the shoulder and neck.
When should I see a specialist?
See a pelvic floor physical therapist or postpartum specialist if:
- You have a gap of 3 or more finger-widths, or a deep, soft tissue defect.
- You're experiencing pain, incontinence, or pelvic organ prolapse symptoms.
- Coning or bulging continues despite doing gentle exercises.
- You're unsure what exercises to do and want a personalized plan (highly recommended).
Getting assessed around 6–12 weeks postpartum is common, but earlier if symptoms are severe. Our team can assess while considering breastfeeding demands — we tailor rehab to feeding schedules, which matters in real life.
How long does it take to recover core strength after diastasis recti?
There's no exact number, but here's a realistic view: many women see meaningful improvement in 8–12 weeks with consistent, targeted work. Full architectural healing of connective tissue may take longer — sometimes 6–12 months — and some people will benefit from continued maintenance training (that's normal).
The best part is — function often improves faster than appearance. You'll likely feel stronger and more able to carry and bond with your baby well before the gap fully closes.
Final tips — practical, not preachy
- Consistency matters: 5–10 minutes, 3 times a day beats one long, exhausting session.
- Quality > quantity: slow, mindful movements rebuild the nervous system and tissue faster.
- Ask for help: hiring a postpartum PT or joining a certified diastasis class can speed progress and reduce anxiety (we can help coordinate that).
- Be kind to yourself: this is healing after major biological work — treat it like rehabilitation, not a quick fix.
Frequently Asked Questions
Can I breastfeed with diastasis recti?
Yes. Diastasis recti doesn't prevent breastfeeding, but it can affect comfort and posture. With proper positioning and gentle core rehab, most people breastfeed successfully.
Will my abdominal separation close on its own?
Sometimes it reduces naturally, but active rehab speeds functional recovery and improves symptoms. Professional assessment helps determine whether conservative care is likely to close the gap or if further interventions are needed.
What signs mean I should stop an exercise?
Stop if you see coning or doming at the midline, feel a sharp pain, or notice increased pelvic pressure (popping, heaviness). If you're unsure, pause and ask a clinician.
Can I wear a belly binder while breastfeeding?
Short-term support during activities (like nursing marathons or heavy lifting) can be helpful, but avoid constant compression. Bind only for comfort and during specific tasks — not as a substitute for rehab.
How do I balance recovery with the demands of a newborn?
Short, frequent sessions (breastfeeding breaks are perfect mini-workouts). Prioritize sleep when you can, accept help, and focus on small wins. If it feels overwhelming, a professional can create a plan that fits your schedule and feeding needs.